Imagine a heart, once a tireless pump, struggling to keep up with the relentless demands of oxygen delivery. This is the reality of heart failure, a chronic condition affecting millions worldwide. The struggle for breath, the fatigue that steals away energy, the constant fear of the next episode – these are the burdens heart failure patients carry daily. Nursing care plans are crucial for supporting these individuals, offering a roadmap to manage symptoms, improve quality of life, and ultimately, extend their years.
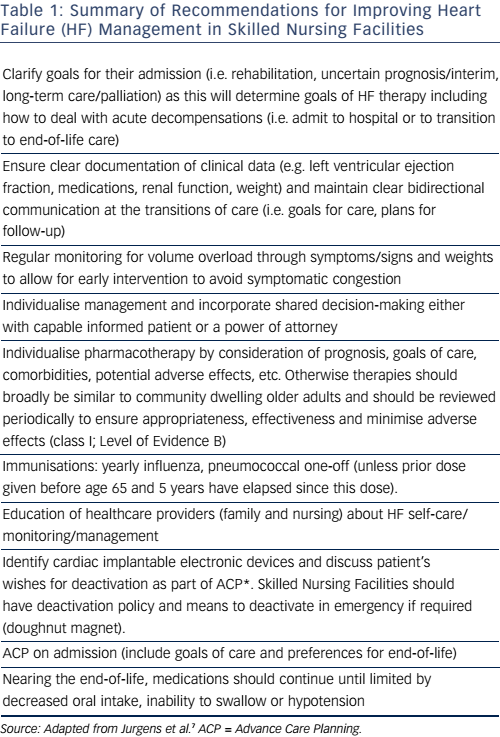
Image: www.cfrjournal.com
This comprehensive guide delves into the core components of a nursing care plan for heart failure. We will explore its purpose, dissect the crucial elements, and provide insights into how nurses can empower heart failure patients to navigate their journey towards better health. Understanding the intricacies of this condition and the vital role of nursing care plans is essential for healthcare professionals, offering them the tools to provide holistic, patient-centered care.
Understanding Heart Failure: A Complex Symphony of the Body
The Heart’s Symphony Gone Awry
Heart failure isn’t a singular disease but rather a complex condition where the heart struggles to pump blood efficiently. This can occur due to a multitude of factors, including coronary artery disease, high blood pressure, valvular heart disease, and congenital heart defects. The heart, once a powerful organ, becomes weakened, unable to meet the body’s oxygen demands.
Types of Heart Failure: Left, Right, and Beyond
Heart failure is categorized based on the side of the heart primarily affected. Left-sided heart failure, the most prevalent type, involves the left ventricle’s inability to adequately pump blood to the body. This results in fluid buildup in the lungs, causing shortness of breath and fatigue. Right-sided heart failure occurs when the right ventricle fails to pump blood effectively to the lungs, leading to congestion in the legs, ankles, and abdomen. While these are the most common types, heart failure can also be classified as systolic or diastolic, depending on the heart’s ability to contract or relax properly.
Image: nurseslabs.com
The Ripple Effect: Complications of Heart Failure
Heart failure’s impact extends beyond the heart itself. The weakened pump can set off a cascade of complications, affecting other vital organs. Fluid overload in the lungs can lead to pulmonary edema, making breathing extremely difficult. The kidneys may struggle to filter waste, causing fluid retention and swelling. The heart’s workload increases, leading to arrhythmias, which can disrupt the heart’s rhythm and further decrease its efficiency. These complications can significantly impact a patient’s quality of life, making comprehensive nursing care crucial.
Crafting the Nursing Care Plan: A Personalized Roadmap
A nursing care plan is not a rigid template but a flexible document that adapts to each patient’s unique needs and goals. It serves as a valuable tool for nurses, outlining the personalized interventions to manage symptoms, promote self-care, and ultimately, improve patient outcomes. This plan involves a multidisciplinary approach, drawing upon the expertise of physicians, pharmacists, and other healthcare professionals.
Assessing the Patient: Unveiling the Underlying Needs
The journey begins with a thorough assessment, gathering information that paints a complete picture of the heart failure patient’s health status. This includes assessing their physical condition, reviewing medical history, conducting a comprehensive medication review, and understanding their emotional and social support systems. Nurses will use established assessment tools like the New York Heart Association (NYHA) Functional Classification, which assesses the severity of heart failure and its impact on daily activities.
Setting Goals: Embracing a Collaborative Approach
Goal setting is a vital step in the care plan creation process. Involving the patient as an active participant in this process fosters their sense of ownership and empowers them to make positive health choices. Goals should be realistic, specific, measurable, attainable, relevant, and time-bound (SMART) to ensure success. These goals may include reducing the frequency of heart failure exacerbations, improving activity tolerance, managing symptoms like shortness of breath and fatigue, and optimizing the patient’s quality of life.
The Nursing Care Plan in Action: Implementing Strategies for Success
Optimizing Medications: A Crucial Component of Management
Heart failure management often involves a complex cocktail of medications. Nurses play a pivotal role in educating patients about their medications, their purpose, and potential side effects. The nurse’s role extends beyond medication administration; they observe for adverse effects, monitor for drug interactions, and collaborate with healthcare providers to ensure the optimal medication regimen for each patient. This includes ACE inhibitors, beta-blockers, diuretics, digoxin, and other medications that help improve heart function, reduce fluid retention, and manage symptoms.
Additional Nursing Interventions: Tailoring Care for Optimal Results
Lifestyle Modifications: Embracing Heart-Healthy Choices
Lifestyle modifications are crucial for managing heart failure. Nurses educate patients on the importance of adopting a heart-healthy diet low in sodium, saturated fats, and cholesterol. Encouraging regular physical activity within their limitations is critical for improving heart function and endurance. Smoking cessation is a paramount recommendation, as smoking significantly exacerbates heart failure. Nurses provide support and guidance to patients as they make these lifestyle changes, addressing their concerns and celebrating their achievements.
Fluid Management: A Crucial Aspect of Heart Failure Care
Fluid management is essential in managing heart failure as fluid overload can lead to complications like pulmonary edema. Nurses monitor daily weight and assess for any signs of fluid retention. They teach patients to measure fluid intake and ensure they are adhering to fluid restrictions. They also highlight the role of daily weights in monitoring fluid balance and identifying potential problems early on.
Monitoring Vital Signs: Unveiling Subtle Changes
Regularly monitoring vital signs is a cornerstone of heart failure care as it provides valuable insights into the patient’s condition. Nurses carefully observe heart rate, blood pressure, respiratory rate, body temperature, and oxygen saturation. Any significant deviations from baseline values can signal potential problems or indicate a worsening of heart failure. Diligent monitoring allows nurses to intervene promptly to prevent complications.
Psychological Support: Empowering Patients to Cope
Living with heart failure can be emotionally challenging. Patients may experience anxiety, fear, and grief. Nurses provide emotional support, helping them cope with the diagnosis, adjust to lifestyle changes, and manage their condition effectively. They encourage patients to express their feelings and explore resources for emotional support. This might include individual or group therapy, support groups specifically for heart failure patients, and community resources.
Patient Education: Empowering Patients to Take Charge
Patient education is paramount in managing heart failure. Nurses play a critical role in educating patients about their condition, its implications, and the importance of adherence to treatment plans. They emphasize self-care strategies like monitoring symptoms, tracking daily weight, and adhering to fluid restrictions. By empowering patients with knowledge, they can actively participate in their care, enabling them to make informed decisions about their health. This involves providing written materials, conducting educational sessions, and using technology like interactive apps to enhance understanding.
The Importance of Collaboration: A Unified Approach to Care
A successful nursing care plan for heart failure requires a strong collaborative effort. Nurses work closely with other healthcare professionals — physicians, pharmacists, physical therapists, social workers, and dietitians— to ensure patients receive comprehensive care. This team approach allows for a holistic view of the patient’s needs, enabling them to address physical, emotional, and social aspects of the condition.
Continual Assessment and Evaluation: Adapting to Changing Needs
A successful nursing care plan is dynamic, not static. Nurses regularly evaluate the patient’s progress, monitor their response to treatments, and make necessary adjustments to the plan. They use patient feedback to identify any areas where the plan needs refinement. This continuous process ensures the plan remains relevant and effective, adapting to the patient’s changing needs and goals.
Embracing Technology: Digital Tools for Enhanced Care
Technology is revolutionizing heart failure care. Remote patient monitoring devices allow nurses to monitor vital signs and assess patient symptoms from the comfort of their homes. Telehealth consultations facilitate communication with healthcare providers, reducing the need for frequent hospital visits. Mobile apps provide personalized information, educational resources, and support networks for heart failure patients. By integrating technology into their practice, nurses can provide more efficient, convenient, and personalized care for patients with heart failure.
Nursing Care Plan Heart Failure Pdf
Conclusion: A Future of Hope and Empowerment
Heart failure is a complex condition, but with comprehensive nursing care, patients can live fulfilling lives. Nursing care plans are the cornerstone of this journey, offering a personalized roadmap for managing symptoms, improving quality of life, and fostering self-efficacy. As nurses, we can empower heart failure patients to actively participate in their care, enabling them to navigate their journey with strength, resilience, and hope. This guide serves as a starting point for understanding the complexity of heart failure and the critical role of nursing care plans. Remember, every heart failure patient deserves tailored, compassionate, and individualized care to help them live a life of quality and dignity.






