Imagine waking up in the middle of the night, struggling to urinate, only to find yourself straining and feeling a burning sensation. This scenario, unfortunately, is a reality for millions of men dealing with prostate enlargement, also known as benign prostatic hyperplasia (BPH). Prostate enlargement doesn’t sound life-threatening, but the discomfort and complications it can cause are quite significant.
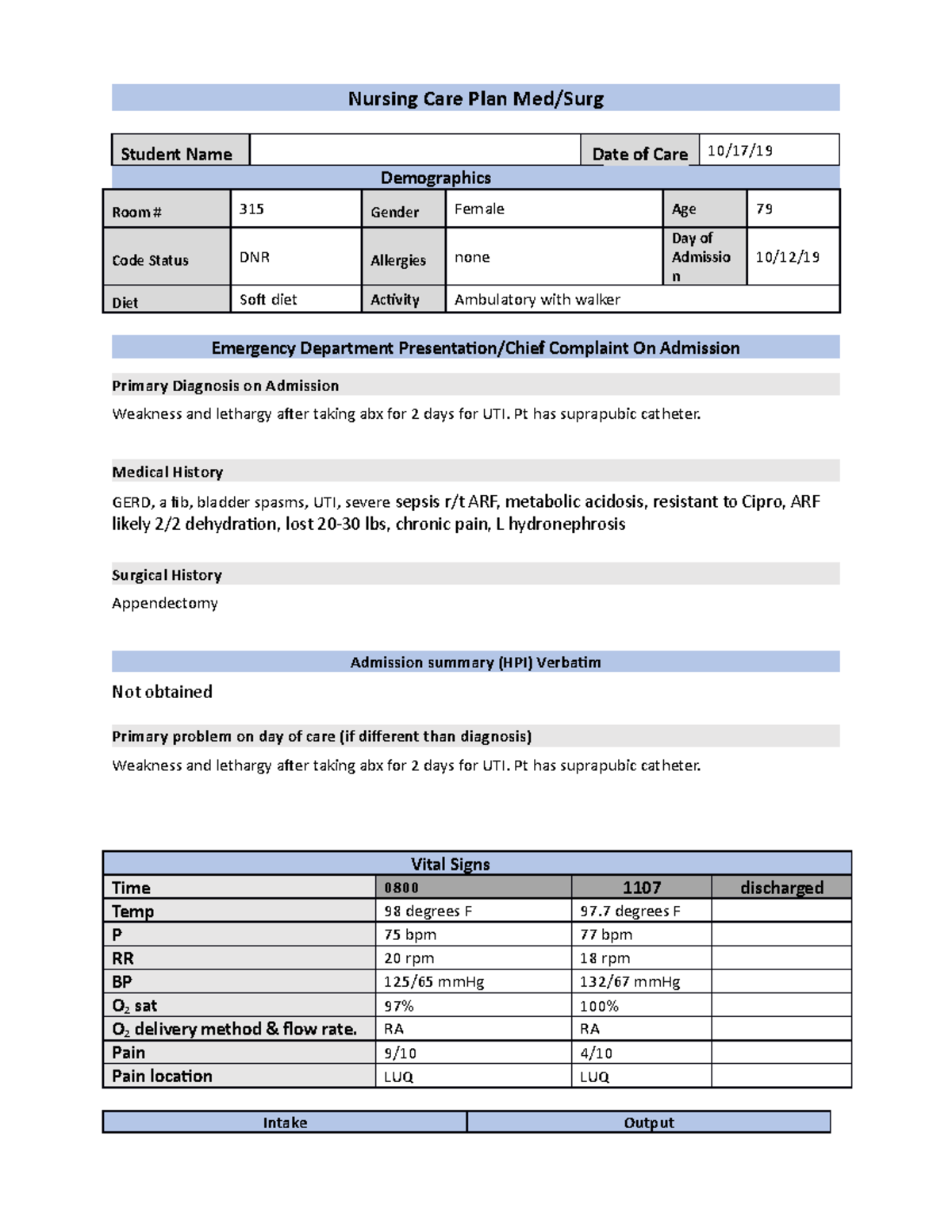
Image: www.studocu.com
This article examines the nursing care plan for patients with prostate enlargement, offering a comprehensive guide for nurses and caregivers. We’ll dive into the intricacies of this common condition, understanding its causes, symptoms, and how nurses play a vital role in managing patient care. By the end, you’ll have a robust understanding of how to provide effective care and support for men facing this challenging health concern.
Understanding Prostate Enlargement
What is the Prostate?
The prostate, a small, walnut-shaped gland situated just below the bladder, plays a crucial role in male reproductive health. It produces a fluid that nourishes and transports sperm. As men age, the prostate often starts to grow, leading to various complications.
What Causes Prostate Enlargement (BPH)?
The exact cause of prostate enlargement remains unclear, but several factors contribute to its development. These include:
- Aging: Prostate growth is a normal part of aging, affecting most men over 50.
- Hormonal changes: Decreased testosterone levels and increased dihydrotestosterone (DHT) levels can contribute to prostate growth.
- Genetics: Family history of prostate enlargement increases your risk.
- Lifestyle factors: Obesity, lack of physical activity, and a high-fat diet are associated with prostate enlargement.
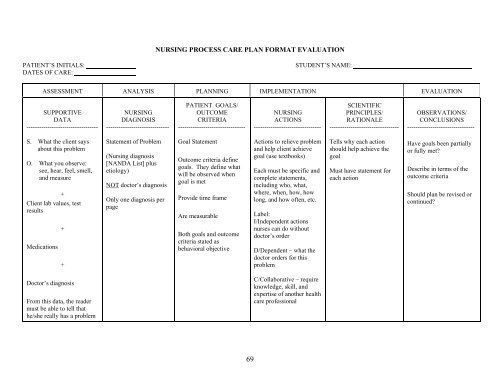
Image: webapi.bu.edu
Symptoms of Prostate Enlargement
The most common symptom of prostate enlargement is difficulty urinating, also known as urinary obstruction. This can manifest in various ways, including:
- Frequent urination, particularly at night (nocturia)
- Weak urine stream
- Hesitancy in starting urination
- Intermittent urine flow
- Straining to urinate
- Feeling of incomplete bladder emptying
If left untreated, prostate enlargement can lead to more severe complications:
- Urinary tract infections (UTIs)
- Kidney stones
- Kidney damage
- Bladder damage
- Urinary incontinence
Nursing Care Plan for Prostate Enlargement
Assessment:
Nurses play a vital role in the early detection and management of prostate enlargement. The initial assessment is crucial to developing an effective care plan.
The assessment should include a thorough medical history, physical examination, and relevant diagnostic tests. This can involve:
- Reviewing the patient’s medical history: Ask about previous urinary issues, family history, and any medications they are taking.
- Performing a physical examination: Palpate the abdomen to check for bladder distention and the prostate gland rectally.
- Ordering diagnostic tests:
- Urinalysis: Detects any signs of infection or blood in the urine.
- Uroflowmetry: Measures the speed and volume of urine flow.
- Post-void residual urine test: Measures the amount of urine remaining in the bladder after urination, indicating bladder emptying efficiency.
- Prostate-specific antigen (PSA) blood test: Helps distinguish BPH from prostate cancer.
- Ultrasound examination: Visualizes the prostate gland and surrounding structures.
- Cystoscopy: Visual examination of the bladder and urethra using a small camera.
Nursing Interventions:
Once the assessment is complete, nurses can implement various interventions aimed at managing symptoms and improving patient quality of life. The goal is to:
- Reduce urinary symptoms
- Prevent complications
- Promote patient education and self-care
Some common nursing interventions include:
- Lifestyle modification:
- Encourage weight loss if the patient is overweight or obese.
- Promote regular physical activity.
- Advise limiting caffeine and alcohol intake.
- Suggest avoiding foods and beverages that irritate the bladder, such as acidic fruits and spicy foods.
- Fluid management:
- Encourage adequate hydration while avoiding large amounts of fluid, especially before bedtime, to reduce nighttime urination.
- Establish a regular urination schedule to aid bladder emptying.
- Medication administration:
- Administer medications prescribed by the doctor, such as:
- Alpha-blockers: Relax muscles in the prostate and bladder neck, improving urine flow.
- 5-alpha reductase inhibitors: Block the conversion of testosterone to DHT, reducing prostate growth.
- Combination therapy: Using two or more medications for optimal symptom control.
- Patient education:
- Provide detailed information about prostate enlargement, its causes, symptoms, and treatment options.
- Teach patients about medication side effects and safety precautions.
- Explain the importance of regular follow-up appointments and monitoring for any changes in symptoms.
- Encourage open communication and address any concerns the patient may have.
- Intermittent Catheterization:
- This technique involves self-inserting a catheter into the bladder to drain urine when the patient is unable to urinate completely.
- Nurses provide education and training for safe and effective catheterization practices.
Surgical Management of Prostate Enlargement
If medical management fails to provide adequate symptom relief, surgical interventions may be considered. These procedures aim to remove or reduce the enlarged prostate tissue, improving urinary flow.
Some common surgical options include:
- Transurethral resection of the prostate (TURP): The most common procedure, involving the removal of excess prostate tissue using an instrument inserted through the urethra.
- Transurethral incision of the prostate (TUIP): This procedure involves making small incisions in the prostate to widen the urethra, improving urine flow.
- Laser prostatectomy: Utilizes a laser to remove prostate tissue, offering minimal invasiveness and faster recovery time.
Nurses play a crucial role in the pre-operative and post-operative care of patients undergoing prostate surgery, advocating for patient safety, overseeing pain management, and ensuring a smooth recovery.
Important Considerations for Nurses
Several factors require special attention when managing patients with prostate enlargement:
- Patient education: Nurses must ensure patients understand their condition, treatment options, and the importance of maintaining a healthy lifestyle.
- Psychosocial support: Prostate enlargement can significantly impact a patient’s quality of life, potentially leading to anxiety, depression, or social withdrawal. Nurses should provide emotional support, encourage open communication, and refer patients to appropriate resources if needed.
- Pain management: Urinary problems associated with prostate enlargement can cause pain and discomfort. Nurses should assess for pain, administer pain medications appropriately, and implement non-pharmacological pain relief strategies.
- Prevention and early detection: Nurses can play a vital role in raising awareness about prostate enlargement and encouraging men to undergo regular prostate-specific antigen (PSA) tests, particularly after the age of 50.
Nursing Care Plan For Prostate Enlargement
Conclusion
Prostate enlargement is a common and manageable condition experienced by many men. Nurses possess the knowledge and skills to provide comprehensive care for these patients, promoting their well-being, alleviating symptoms, and preventing complications. By understanding the intricacies of the condition, implementing effective nursing interventions, and advocating for patient education and psychosocial support, nurses are empowered to play a significant role in improving the quality of life for men dealing with prostate enlargement.
Remember, open communication with your patients is vital. Listen to their concerns, address their questions, and involve them in their care plan. Together, we can empower men to manage prostate enlargement and live fulfilling lives.






